 #News
#News
More patient-centric clinical trials
Decentralized research helps to widen the diversity of patients undergoing clinical trials and expedite the development of new medications and therapies
 More than 10,000 clinical trials have been conducted in Brazil, leading in Latin America with 42% of the total, but representing only 2% globally according to the database ClinicalTrials.gov | Image: Shutterstock
More than 10,000 clinical trials have been conducted in Brazil, leading in Latin America with 42% of the total, but representing only 2% globally according to the database ClinicalTrials.gov | Image: Shutterstock
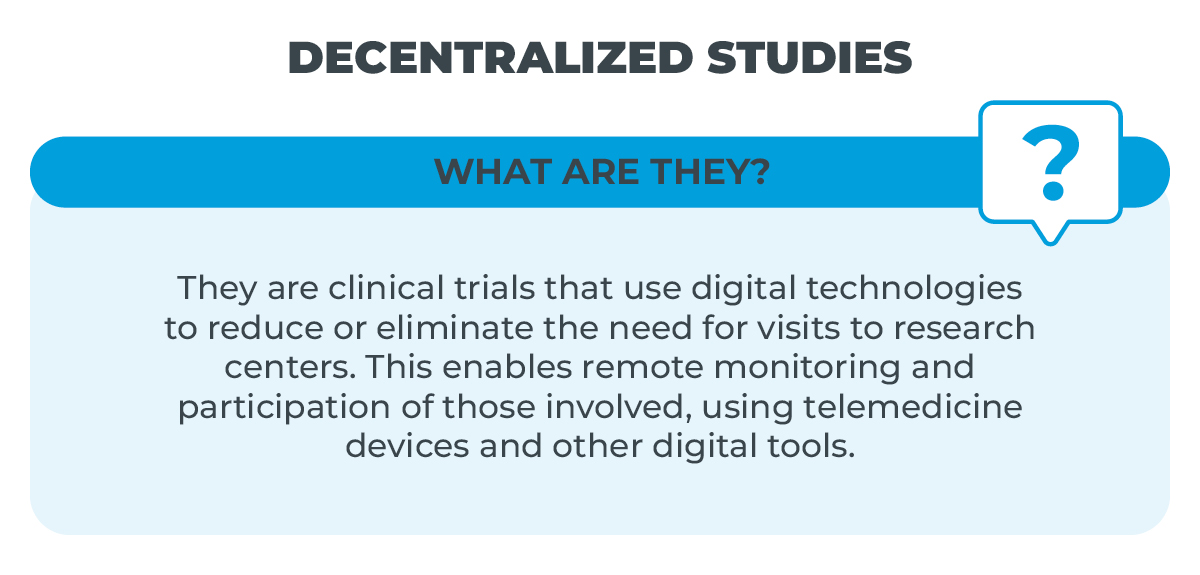
In recent years, decentralized clinical trials (DCT) have gathered momentum with the proposal to transform the way in which medical research is conducted.
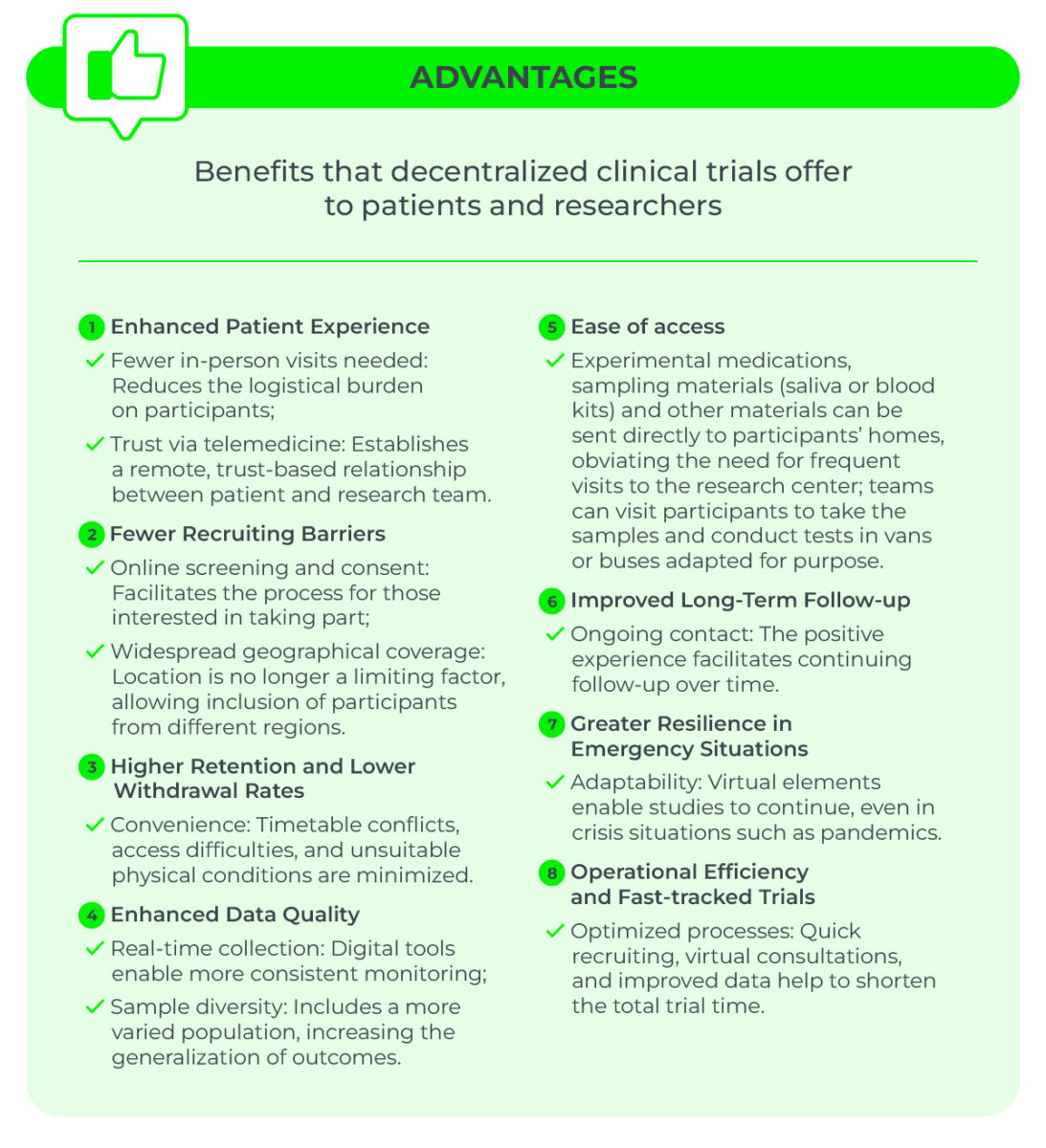
Unlike traditional clinical trials, in which all processes are centered at research facilities, decentralized approaches have the potential for breaking down geographical barriers and widening patient access to studies into the safety and efficacy of new medications and treatments.
This is thanks to the increasing use of digital trial management platforms, enabling patients to take part without leaving home.
This approach may contribute to reducing clinical trial costs, increasing ethnic diversity among the volunteers, and streamlining data collection.
But how to ensure safety, quality, and participant buy-in to a relatively new methodology on a global scale? Specialists interviewed by Science Arena highlight the advantages and advances shaping the future of clinical trials in Brazil and around the world.
Regulatory frameworks
The COVID-19 pandemic contributed to more widespread dissemination of the concept of decentralized clinical trials, and implementation of new access components to facilitate the participation of volunteers engaging in the testing of potential new treatments.
Regulatory adaptations for acceptance of decentralization processes was another plus point for clinical trials to continue, even during the lockdowns and movement restrictions imposed by the pandemic.
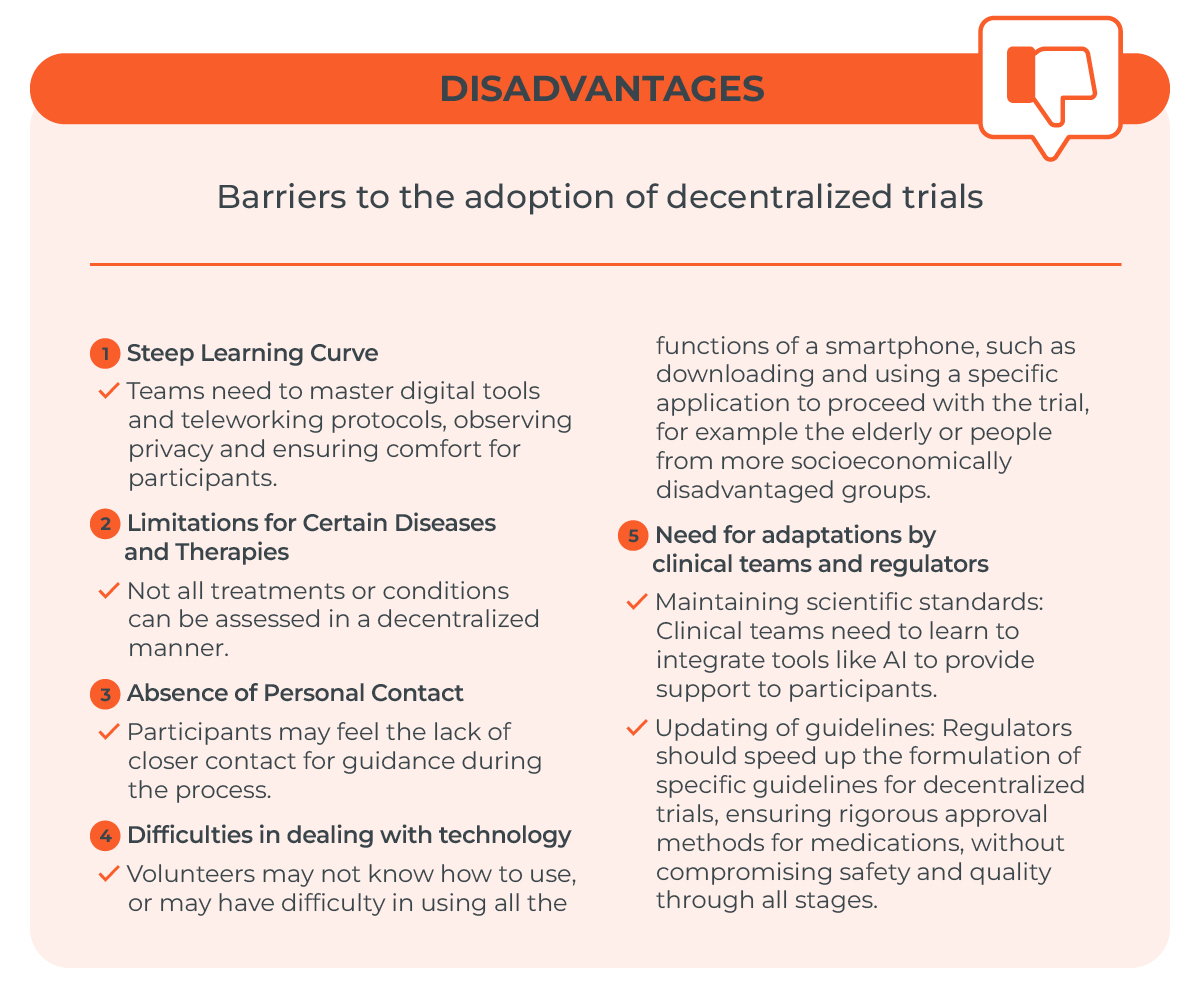
“At the time, we had more relaxed rules on patient access to decentralized clinical trials, but that is currently no longer the case,” explains Fernando de Rezende Francisco, executive director of the Brazilian Association of Clinical Trial Representative Organizations (ABRACRO).
He says that during the pandemic, the Brazilian Health Regulatory Agency (ANVISA) disclosed resolutions to facilitate the progression of certain clinical trials, so that the tested medication would be shipped to participants’ homes and remote consultations would take place.
“At the end of the pandemic, however, the regulators saw that the market, or indeed they themselves, were not fully prepared to analyze and adapt themselves to these rules in a normal routine,” says Francisco.
He states that specialized clinical trial companies are applying considerable pressure for trials to be conducted more quickly, widening the patient participation base, and thereby increasing the volunteer retention rate.
“If, on one hand, Brazilian potential is driven by its genetic diversity, on the other, regulation slows the trial approval rate, an essential factor for attracting more international multicentric trials,” says Francisco.
A spokesperson for ABRACRO says that regulatory advances can also have significant economic impacts, “with the potential for generating investment of around R$3 billion per year.”
Bright future
“Brazil and the wider world are still learning how to conduct decentralized trials,” says Karla Espírito Santo, head of Decentralized Studies and New Clinical Trial Models at Hospital Israelita Albert Einstein’s Academic Research Organization (ARO).
“In specific cases of trial phases for approval of new medications, in which the controls are stricter, regulators are still adapting and signing off on guidelines to assist in this process and maintain the high standards of clinical trials,” explains the researcher.
Inspired by international research institutions, projects at ARO-Einstein fully encompass clinical trial management, from the planning phases—with formulation of the protocol and regulatory approval process—through conduct of the study, to statistical analysis.
The ARO also discloses outcomes through presentations at national and international medical conferences, and by publishing in high-impact scientific journals.
Logistical challenges
Achieving more decentralized clinical trials in Brazil comes with added logistical challenges in the shipping of medications, says Laura Melgarejo-Herrera, director of Latin America Business Development for Care Access, a US company that specializes in decentralized clinical research.
“Brazil is a country of continental proportions, and for this reason we have made progress in optimizing the reach of the healthcare network and the logistics for distribution of supplies to the research centers and their participants, primarily in remote regions where access to scientific institutions is challenging,” explains Melgarejo-Herrera, who sees the decentralized model as an effective tool in countries such as Brazil and across Latin America as a whole. “Not only because it enables identification of different populations with the potential to participate in clinical trials, but also because it helps to widen access to innovative treatments.”
“The use of artificial intelligence and real-time integrated systems is our ally in this mission,” continues Melgarejo-Herrera. Moreover, she says, such technologies improve the quality of trial data, “with the patient always the central focus of our attention.”

Herrera explains that, through its network of research centers and mobile units, Care Access can identify potential clinical trial participants to achieve more comprehensive patient representation.
This approach is aimed at speeding up approval of new therapies and increasing treatment options for more patients. “Decentralization can also help to raise standards of quality in clinical research and provide more diversity among participants,” highlights the biomedical scientist.
Technological obstacles
Technological barriers also hamper efforts to increase the number of participants in decentralized clinical trials, primarily among sections of the population with poor levels of education and the elderly.
“Technologies developed over recent decades help us in this process, but low levels of literacy among participants is a challenge for sign-up,” says Karla Espírito Santo, of Einstein.
“Volunteers will have smartphones and know how to use message apps, but they are often unable to download a new application without help—sometimes, not even when they have remote assistance.”
Increasing the offer of decentralized trials among this section of the population—with low or even nonexistent levels of digital literacy—can stimulate new inclusion initiatives.
Adaptation strategies for the use of technology such as WhatsApp, to facilitate the completion of forms and send explanatory videos, or the creation of a chat space to address one-off technological issues, are also planned by the Einstein researchers, says Espírito Santo.
“The technical side needs to be constantly updated to avoid, or more quickly fix, certain bugs,” says the researcher.
“Another solution would be to segment the use of technologies for certain participant groups,” she suggests.
“For example, having a group of participants more familiarized with new technologies assuming responsibility for operating the app, with another group exchanging information by telephone,” she proposes.
Physician Julia Machline, head of medical affairs at startup epHealth, believes this to be merely a cultural issue, and not effectively an obstacle. “There is no single recipe for all the countries; There are nuances to be analyzed. For example, in the UK, the most frequently used means of communication is SMS or telephone call, not WhatsApp, as is common in Brazil.”
The Brazilian researcher, who lives in London, is also a volunteer in a decentralized trial: Our Future Health is a large-scale observational study being conducted across the UK, with an end to improving cardiovascular prevention among the population.
Machline signed up via the website, and received correspondence from the UK National Health Service (NHS), with a form for information on her health background and lifestyle.
The collection of samples for data, such as blood, weight, and blood pressure was carried out close to her home at a partner pharmacy, which then submitted the results to the public health system.
“I had no direct contact with any researcher,” recounts Machline. “It was very interesting to take the standpoint of a participant in a clinical trial, and not just of a researcher.”
Growing room and ethnic diversity
According to data from ABRACRO, more than 10,000 clinical trials have been conducted in Brazil, accounting for 42% of the total in Latin America. Although at the forefront regionally, the country represents only 2% of clinical trials on the world stage.
With a multiethnic population of more than 200 million, and different regional climates, Brazil has enormous potential to become a reference in clinical trials.
Approval was recently granted for Law no. 14.874 of 2024, setting out a new regulatory framework for clinical trials with humans by public and private institutions, and bringing significant advances for the area.
“It is expected that this group will start to grow in 2025, and possibly in 3 to 5 years Brazil will account for 5% of clinical trials conducted globally, featuring among the 10 leading countries in the world,” predicts Francisco, of ABRACRO.
“Brazil is a great center for clinical trials due to its ethnic diversity and genetic miscegenation.”
Its ethnic and cultural diversity is, without doubt, the “crown jewel” of clinical research in Brazil.
A large proportion of clinical trials published currently present at least 65% white Caucasian participants.
By contrast, data from the 2022 Census conducted by the Brazilian Institute of Geography and Statistics (IBGE) indicate that more than 45% of the country’s population is made up of people declaring as nonwhite; the pressing need to increase participation among Indigenous, mixed-race, and Black people in clinical trials positions Brazil as a hotbed of ethnic diversity in this type of research.
These groups, historically underrepresented in scientific studies in Brazil and around the globe, face barriers to access and inclusion that limit the diversity of data found.
Thus, increased participation by these sections of society is paramount to ensure that the outcomes of clinical trials are a more representative cross-section of the population as a whole.
Moreover, such heightened involvement can improve the efficacy of treatments and interventions for different ethnic groups, considering their genetic and socioeconomic characteristics.
Expanding inclusion criteria, which generally exclude the over-60s and make it difficult for older people to access trials (which also happens with the pediatric community), is another factor to be reexamined in studies.
“The idea is to increase the diversity of participants in clinical trials, and not just among the small group of patients already attending research centers,” emphasizes Karla Espírito Santo.
*
This article may be republished online under the CC-BY-NC-ND Creative Commons license.
The text must not be edited and the author(s) and source (Science Arena) must be credited.
News
 #News
#News
 #News
#News
 #News
#News
