 #Essays
#Essays
Immunotherapy using checkpoint inhibitors brings new hope to many cancer patients, but there is a need for improvement
Research focuses on understanding immune mechanisms behind anti-tumor immune responses in oncology patient volunteers
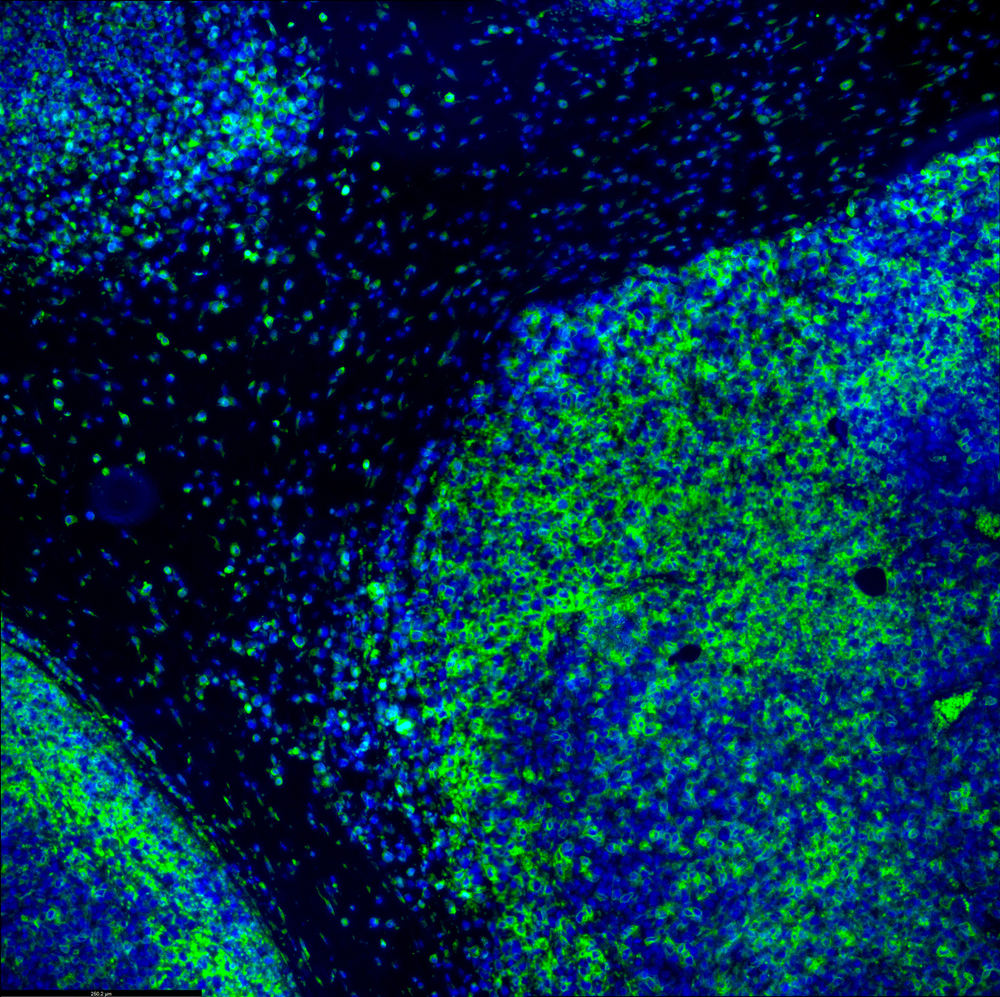 Tumour immunofluorescence IHC image of immunotherapy treatment. | shutterstock.com
Tumour immunofluorescence IHC image of immunotherapy treatment. | shutterstock.com
Cancer presents a significant global health challenge, and in Brazil, the National Cancer Institute (INCA) estimated an annual diagnosis of 704,000 new cases between 2023 and 2025. Traditionally, cancer treatment relied on three pillars: surgery, radiation therapy, and anti-cancer drugs until the advent of immunotherapy in 2014. This novel approach, leveraging treatments that reactivate an inhibited immune response to attack tumors, marked a new era in cancer care. Immunotherapy, particularly through checkpoint inhibitors — antibodies that unleash the immune system to attack tumors — brought renewed hope to patients with advanced stages of cancer and earned Drs. James Allison and Tasuku Honjo, basic science researchers, the Nobel Prize for Medicine in 2018.
These pioneering researchers delved into understanding T cell biology, and their late 1990s discoveries led to the development of the first classes of immune checkpoint inhibitor therapies, which activate the immune response in cancer patients to combat tumors. Dr. Allison’s work led to the creation of anti-CTLA-4, and Dr. Honjo’s to anti-PD-1, both molecules that, when inhibited, reactivate a suppressed immune response to target tumors. In clinical settings, the combination therapy of anti-PD-1/anti-CTLA-4 witnessed a remarkable surge in the percentage of metastatic melanoma patients reaching a 5-year survival rate, from 10-20% with chemotherapy to 52%. Similarly, metastatic lung cancer patients experienced a substantial escalation in the 5-year overall survival rate, increasing from 9.7-11.3% with chemotherapy to 18.4-19.4% with anti-PD-1 plus chemotherapy. Notably, among the subgroup of patients who completed 2 years of therapy, 71.9% were still alive after 5 years.
While these numbers are impressive and represent a major improvement for cancer treatment, a significant proportion of patients remain unresponsive, and several cancer types lack effective immunotherapies. Thus, our research focuses on understanding immune mechanisms behind effective versus inefficient anti-tumor immune responses in oncology patient volunteers. Our goal is to discover and validate novel targets for expanding the use of immunotherapy to combat other tumor types and increasing the percentage of cancer patients that respond to therapy. There is a dynamic interaction between the immune response with a cancer and, in some cases, the cancer can inhibit and suppress the immune response’s ability to kill cancer cells. In these cases, the tumor can grow and spread to other tissues. By identifying the mechanisms (molecules, pathways or cells) behind suppression of anti-tumor immune response, we aim to develop targeted therapies to reignite the immune system’s tumor-fighting capabilities. In collaboration with clinical teams and researchers at Hospital Israelita Albert Einstein (HIAE), Hospital Vila Santa Catarina, and A.C.Camargo Cancer Center, we study the immune response in cancer patient volunteers. This involves analyzing blood samples and tumor fragments removed by the patient’s surgeon during cancer treatment.
In recent studies, we have identified immune cell subpopulations and soluble mediators that are increased in the blood of patients that do not respond to immunotherapy checkpoint inhibitors. With this finding, we can now study ways of inhibiting or blocking these components to favor the reactivation of an anti-tumor immune response. In addition, we work to discover potential biomarkers that can identify patients that have the best chance of benefiting from immunotherapy. We look for blood markers that predict which patients will respond to therapy and those most likely to not develop severe adverse events (negative side effects). This approach not only improves patient outcomes but also reduces costs and enhances accessibility to immunotherapies through public healthcare networks, such as the Brazilian unified health system (SUS).
In conclusion, these studies are performed in the Translational Immuno-oncology Laboratory at HIAE, within the newly established Center for Research in Immuno-oncology (CRIO), with the collaboration of patient volunteers and multidisciplinary research teams including clinicians, surgeons, nurses, radiologists, pathologists, researchers, graduate students and other professionals. CRIO was established in 2022 via funding by FAPESP and the pharmaceutical company GSK, along with major investments from HIAE. The center is composed of HIAE (host institution), Hospital Vila Santa Catarina, A.C.Camargo Cancer Center and Ribeirão Preto Medical School (University of São Paulo).
To learn more about immuno-oncology and follow CRIO’s research, visit the website (https://crio.einstein.br/) and follow the Imuno Agentes podcast (in Portuguese) on the main audio platforms: Spotify, Google Podcasts, Castbox e Amazon Music.

*Kenneth J. Gollob is an immunologist, director of the Center for Research in Immuno-oncology (CRIO), Head Translational Immuno-oncology Laboratory at Hospital Israelita Albert Einstein
*
This article may be republished online under the CC-BY-NC-ND Creative Commons license.
The text must not be edited and the author(s) and source (Science Arena) must be credited.


