#Columns
#Columns
Preparing For the Next Global Challenges: The Ebola vaccine example
Developing and manufacturing vaccines that have a global impact requires working with global partners, focusing on delivering real solutions to the ongoing threat of the next pandemic
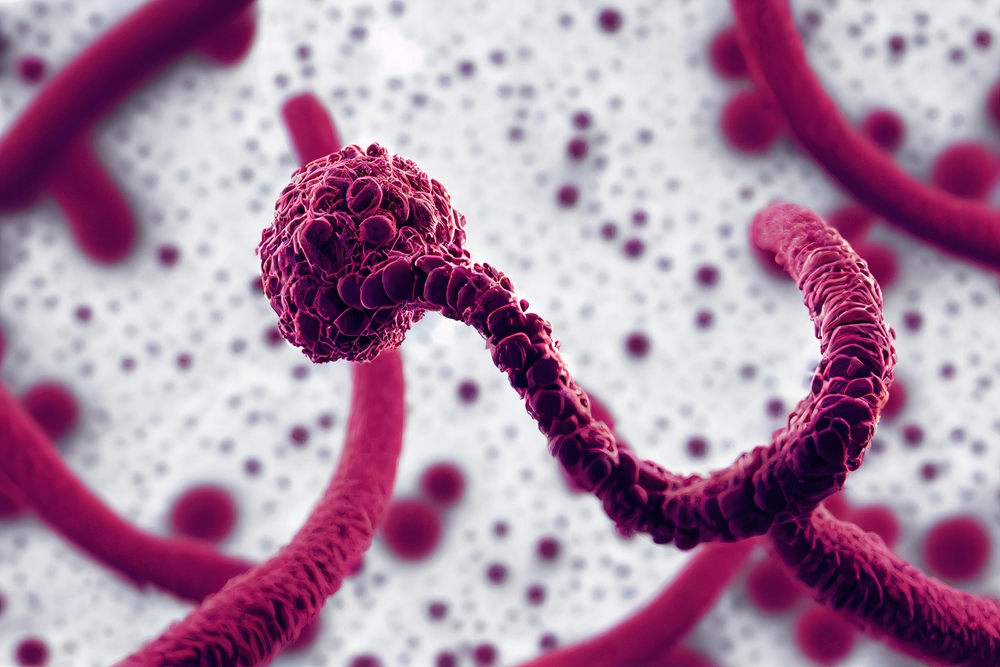 A virus of the Filoviridae family, the Ebolavirus was discovered in 1976, from outbreaks that occurred in southern Sudan and northern Democratic Republic of Congo, near the Ebola River, which gives the virus its name.
A virus of the Filoviridae family, the Ebolavirus was discovered in 1976, from outbreaks that occurred in southern Sudan and northern Democratic Republic of Congo, near the Ebola River, which gives the virus its name.
There exists an urgent unmet need to develop and test vaccines and therapeutics against emerging and outbreak pathogens and to define rapid, scalable and deployable solutions through which these vaccines and therapeutics are used.
In September 2022, Uganda declared the first Ebola outbreak in a decade, caused by Sudan ebolavirus (SUDV). Soon after, two separate outbreaks of Marburg virus were declared in Equatorial Guinea and Tanzania and more recently in Rwanda.
The disease, named after the Ebola River Valley which is the site of its first outbreak in 1976, Ebola virus is a filovirus that causes haemorrhagic fever and is associated with a high mortality rate.
There are five well-known species in the genus: Zaire ebolavirus, Sudan ebolavirus, Taï Forest ebolavirus (previously named Côte d’Ivoire), Reston ebolavirus, and Bundibugyo ebolavirus, discovered in 2007.
Sudan ebolavirus survives in wild animals and humans are frequently infected via animal exposure.
Long-standing concern
Marburg virus (MARV), another member of the filovirus family, has been a major concern since 1967, causing many outbreaks in sub-Saharan Africa, with two major ones in 1998 and 2004.
There is a single species of Marburg – Marburg Marburgvirus. Human infection with MARV usually results from prolonged exposure to infected Rousettus bat colonies, and similar to EBOV and SUDV, its infection causes severe haemorrhagic fever, organ failure and death.
Although less frequent than Zaire ebolavirus (EBOV), SUDV infection displays similar symptoms as EBOV, with a mortality rate of 55%. Marburg virus disease can have a fatality ratio of up to 88%.
Control is primarily achieved through community engagement surveillance, contact tracing and case management, as well as risk communication.
The most recent outbreak in Rwanda (October 2024) highlights the serious public health threat that transmission of a filovirus represents.
The high number of fatalities and the potential for rapid spread into the community, mean that the development of vaccines and therapies remains a high priority.
o inicial do tratamento em várias áreas importantes.
A number of vaccines against ebolavirus (originally called Zaire ebolavirus) have been licensed for use.
These vaccines include viral vector platform technologies, some of which demonstrated efficacy during the West Africa 2013-2015 outbreak and others which were licensed by the ‘animal rule’.
There are no licensed vaccines against Sudan Ebolavirus or Marburg virus.
However, the ChAdOx1 platform technology, which was successfully used during the covid-19 pandemic, represents a feasible solution to generating a vaccine against filoviruses.
Effective platform
When compared to other technologies, the ChAdOx1 platform responds well to high demand, high volume, low cost, global storage conditions and the need for fast deployment in a pandemic situation.
This platform is highly immunogenic, eliciting an immune response both cell mediated, specifically CD8 + T cell response, and humoral immune response.
Other equally important advantages are:
- Speed;
- Ease of manufacture and scale-up;
- Ease of deployment;
- Technology transfer to other manufacturers to ensure worldwide supply;
- Cost of goods.
The ChAdOx1 nCoV-19 vaccine was approved or granted emergency authorisation in approximately 100 countries, and had over 20 partners collaborating on its manufacture.
This resulted in more than 3 billion doses released for supply in more than 180 countries and an estimated > 6 million lives saved in 2021 alone.
Working with global partners is the best approach to generating enough vaccine to make a global impact.
During the filovirus outbreaks in 2022 and 2023, candidate filovirus vaccines designed and progressed by Professor Lambe’s team at the University of Oxford were shortlisted by the WHO Technical Advisory Group on candidate vaccine prioritization (TAG-CVP) for inclusion in ring vaccination protocols to combat the outbreaks.
Prof Lambe and team, based in the Pandemic Sciences Institute and Oxford Vaccine Group, worked with partners to rapidly scale vaccine production generating more than 300,000 doses of the vaccine.
They filled 40,000 doses less than 80 days from receiving the starting material for the candidate vaccine against the Sudan ebolavirus outbreak strain. Global partnerships, working closely with the WHO and the relevant ministries of health, offers real-world solutions to the continued threat of the next pandemic.
The Covid-19 pandemic demonstrated that a more rapid vaccine development and deployment pathway is needed and given that experience, we are in a unique position to make real change and to better prepare for the next outbreak.

Sue Ann Costa Clemens is Head of the Institute for Global Health at the University of Siena, where she is Director of the Masters Program in Vaccinology and Drug Development and Professor of Pediatric Infectious Diseases. She is a Global Health and Clinical Development Professor at the University of Oxford, Director of the Oxford Latam Vaccines Group, and Professor and International Scientific Coordinator at the Carlos Chagas Institute. She has been a Senior Advisor to the Bill and Melinda Gates Foundation since 2012 and is a member of scientific advisory boards at several institutions. In 2023, she was a World Health Organization Expert Group on Access and Information on Vaccines (TAG-MI4A) member. She has contributed to developing more than 20 globally licensed vaccines and medicines over a career spanning more than 25 years. Sue Ann was awarded the Order of the British Empire, CBE, by Queen Elizabeth II for services to Public Health; she is also a Commander of the Federative Republic of Brazil in the Orders of Rio Branco and Medical Merit.
Opinion articles do not necessarily reflect the views of Science Arena or Hospital Israelita Albert Einstein.
*
This article may be republished online under the CC-BY-NC-ND Creative Commons license.
The text must not be edited and the author(s) and source (Science Arena) must be credited.