 #News
#News
Some 350 children die from congenital syphilis in Brazil every year
According to a study, deaths can be avoided with simple, inexpensive treatment during pregnancy
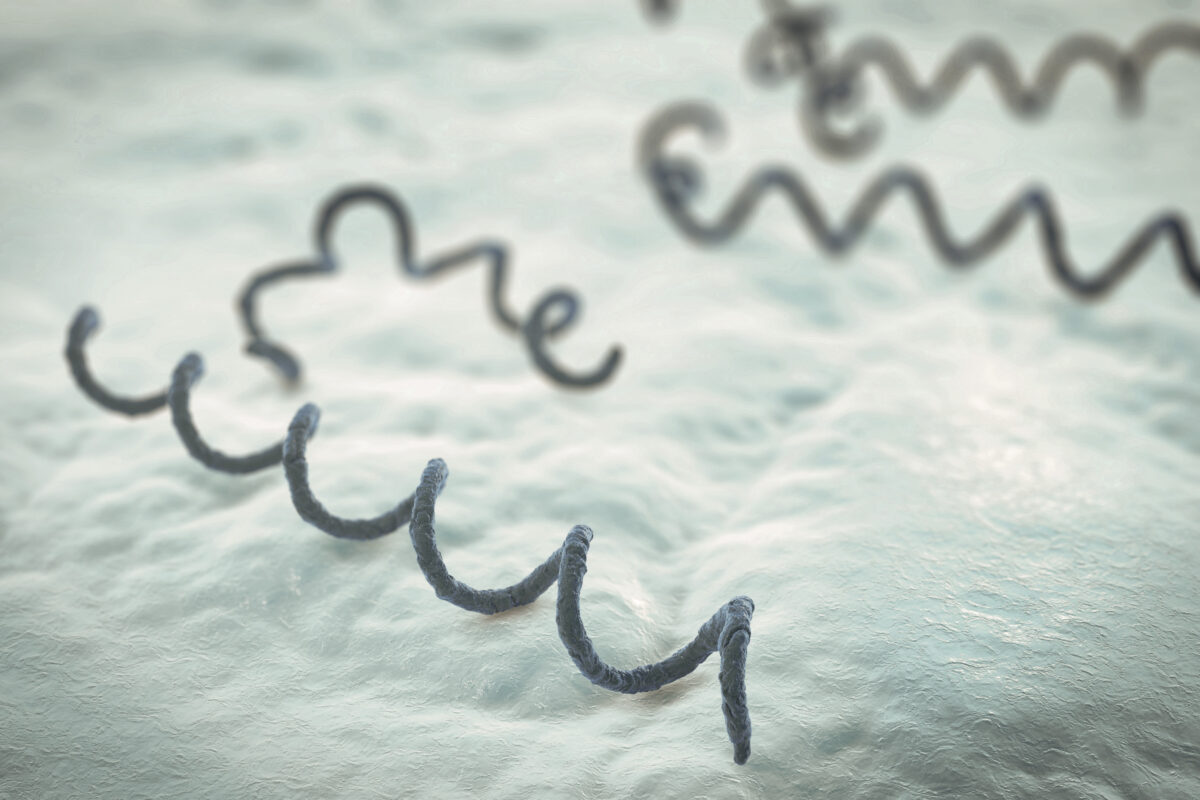 Congenital syphilis is caused by transmission of the bacteria Treponema pallidum from mother to fetus via the placenta or during childbirth | Illustration: Shutterstock
Congenital syphilis is caused by transmission of the bacteria Treponema pallidum from mother to fetus via the placenta or during childbirth | Illustration: Shutterstock
Between 2011 and 2017, some 350 children died per year from congenital syphilis in Brazil, a disease that can be avoided by treating the infection in the expectant mother with penicillin. Among babies born with the disease, the risk of death was almost 2.5 times higher than among the others. The numbers were compiled based on data from the Brazilian Unified Health System (SUS) and presented in an article published in the journal Plos Medicine.
“This is a ridiculously high number considering that treatment of expectant mothers is relatively simple and cheap,” says epidemiologist Enny Paixão Cruz of the Oswaldo Cruz Foundation (FIOCRUZ) in Bahia State, one of the article’s authors. Cruz observes that in the UK, where she is a visiting researcher at the London School of Hygiene & Tropical Medicine, there are fewer than 10 deaths per year.
Congenital syphilis is caused by transmission of the bacteria Treponema pallidum from mother to fetus via the placenta or during birth. The mother normally contracts the disease during unprotected sex or through contact with contaminated blood. Newborn babies may present serious symptoms such as poor bone formation, hearing impairment, slow mental development, among other issues, or may be born without any apparent symptoms and develop them in the first two years of life.
Researchers verified that some 20 million children were born in Brazil between January 2011 and December 2017. Of these, approximately 93,500 were diagnosed with congenital syphilis at birth, and 2,500 died. The majority of these deaths (33%) occurred in the neonatal period—within 28 days of birth; 11% occurred between one month and one year, and 3% from 1 to 4 years. The risk of death compared to babies without the disease was almost 9 times higher in those born with a high concentration of antibodies against the syphilis bacteria, indicating acute infection, and 7 times higher in those born with symptoms.
To obtain these results, researchers cross-referenced three SUS databases: the Live Birth Information System (SINASC), which registers births, the Mortality Information System (SIM), which carries data on deaths, and the National Notifiable Disease System (SINAN). This study was possible because health centers are obliged to report identified cases of congenital syphilis to SINAN.
“The study is very sophisticated as it involves complex databases,” states nursing professor Mellina Yamamura Calori of the Federal University of São Carlos (UFSCar), who did not take part in the study.
Calori agrees that the data are alarming, and states that the problem needs to be addressed on multiple fronts. “Transport for mothers and their companions needs to be facilitated, increasing available attendance hours and tackling the stigma,” she adds.
The real harm caused by the disease, however, is even greater than that calculated by the study. As SINASC registers the birth of live babies only, the total number of deaths calculated in this study does not include abortions and stillbirths.
Care failures
Causes of these high fatality numbers vary. One of them, according to Cruz, is that the results of the exam that detects the presence of antibodies against the bacteria which causes syphilis, known as VDLR, applied routinely to expectant mothers, can take up to 3 months to return. Therefore, the result often arrives after the cut-off for commencement of treatment, which must begin more than one month before birth.
Even when the diagnosis is made within the timeframe and the expectant mother is treated, the woman’s partner does not always go along with the treatment, which can cause reinfection. Although the stigma of this disease can contribute to low levels of take-up by men, health center opening hours, between 8 a.m. and 5 p.m. only, make getting treatment difficult for those working all day.
Another issue arises when the baby is born: difficulties in diagnosing the disease. The result of VDLR testing on the baby is not a precise indication of congenital syphilis, as antibodies transferred from the mother can remain in the blood even if the newborn is not infected. The tendency is for the concentration to be higher in the case of infection, and lower when it has been eliminated, but there is no way of being certain.
For this reason, the blood test result is interpreted based on other information, particularly if the mother was treated within the timeframe and if the baby was born with symptoms—some of which, such as jaundice and nasal secretions, are not specific to congenital syphilis but may contribute to the diagnosis. In some cases, however, symptoms such as low weight and respiratory issues only arise during the first two years.
Additionally, from 2014 to 2016, fabrication of penicillin, used to treat the disease, was interrupted due to it being an inexpensive medication and not prioritized by the pharmaceutical companies, according to Cruz. “The main risk factors are the low level of education, single mothers, and the socioeconomic situation,” she says.
Another problem is that penicillin can cause anaphylaxis, an acute allergic reaction, which is treated with adrenaline. Often, as a precaution, health centers that do not have this medication do not apply the treatment. “The percentage of problems caused by penicillin is very low, while lack of treatment for congenital syphilis causes enormous harm,” adds Cruz.
Calori, from UFSCar, agrees that the number of deaths is excessive and notes that with public health policies having been dismantled during the pandemic, the number could rise in the coming years. “Expectant mothers and their partners were not properly treated during this period,” she states.
*
This article may be republished online under the CC-BY-NC-ND Creative Commons license.
The text must not be edited and the author(s) and source (Science Arena) must be credited.


